Most people who go to the podiatrist would never expect to get biopsied and diagnosed with a rare, dangerous skin cancer. But that’s exactly what happened to Dorothy Overstreet in 2020, during the height of the COVID-19 pandemic. Now, she wants to educate people about acral lentiginous melanoma (ALM) and how to detect it.
Dorothy, who was 76 at the time, was getting a corn removed when her podiatrist noticed a dark patch of skin on her left heel.
“My doctor said, ‘What’s that? Do you mind if I biopsy it?’”
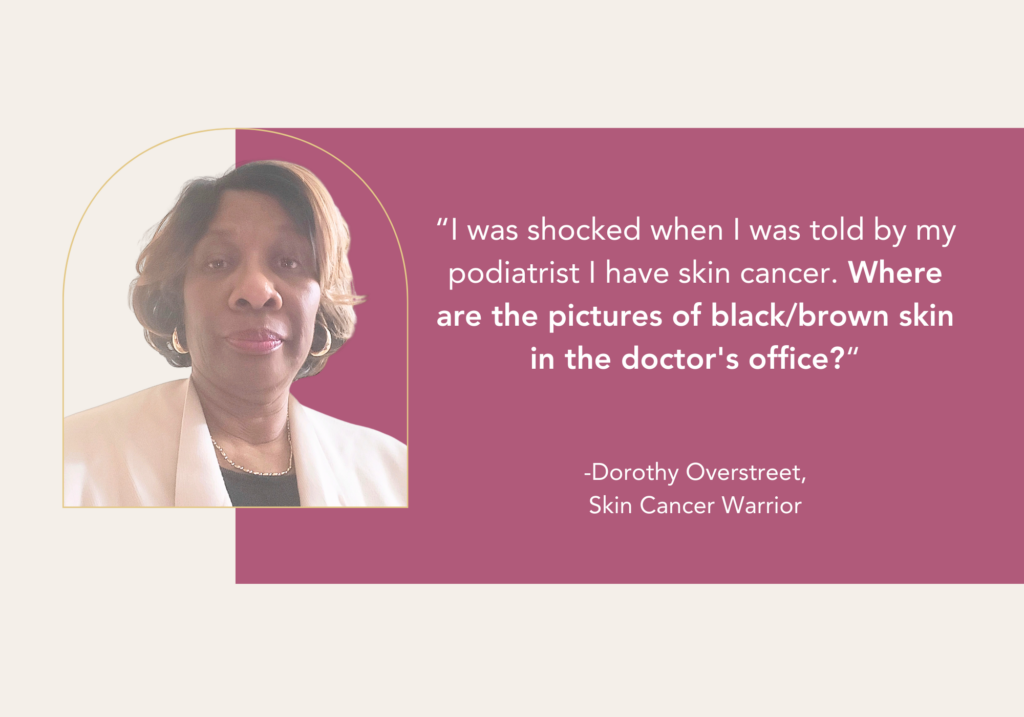
She was shocked to hear that he suspected a melanoma. “I told him, ‘But my foot’s not in the sun and my skin is not white.’” Dorothy explained. “That’s when I realized that anyone can get skin cancer.”
Eight days later, her doctor delivered the news: Dorothy had acral lentiginous melanoma and needed immediate surgery. View her video.
In an instant, her life took a new and frightening turn. Dorothy took the rest of the day off to process the news. “I never heard of melanoma on the foot. Then I researched and read about Bob Marley,” she said.
Following her podiatrist’s orders, Dorothy booked a consultation with a dermatologist and a plastic surgeon.
About ALM
ALM is the most common melanoma found in people of color. It often appears as a black or brown discoloration on the palms of the hands, soles of the feet or under the nails. If left untreated, it can grow and spread to other parts of the body. Recognizing the early warning signs can make the difference between life and death.
For people of color, ALM and other skin cancers are often diagnosed later, when they become more challenging to treat. This delay in diagnosis is attributed in part to a lower public awareness of the risk of skin cancer among people of color. And because the chances of skin cancer are smaller in patients of color, there’s often a lower index of suspicion among health care providers. And third, the places on the body where skin cancers tend to occur in people of color are often in less sun-exposed areas, making detection more difficult.
Flap Surgery and Reconstruction
Dorothy got some good news before her surgery: the pathology report showed that the melanoma had not spread beyond the original tumor site, and her lymph nodes were clean.
At her consultation, the doctors explained that after the melanoma was removed, Dorothy would undergo flap surgery so that she would be able to walk again. While physicians commonly use wide excisional surgery to remove acral melanoma, the location and size of Dorothy’s tumor required flap surgery to fully reconstruct the site using surrounding tissue.
“I brought a notebook and drew pictures of what the doctors were explaining to me,” she said. “And I put my trust in these doctors.”
Nine days later, Dorothy had a three-hour operation. Her surgeon removed the melanoma, then took a graft of tissue from her inner leg to repair her foot.

Stage II acral lentiginous melanoma on Dorothy’s left foot. Photo courtesy of: Dorothy Overstreet

Surgical reconstruction of Dorothy’s foot
A Long, Challenging Recovery
When she came home from the hospital with heavily bandaged foot and leg, Dorothy was given strict orders against bearing any weight. She had to stay in bed or on the sofa with her foot elevated. Thankfully, her daughter, a nurse, took time off to change her dressings each day for the first two weeks.
Recovery was a long, difficult journey. Three months of being immobilized, alongside the isolation and fear associated with the pandemic took its toll on Dorothy’s mental health.
“It was a frightening experience. I had anxiety, depression, PTSD and paranoia,” she explained. “I thought, ‘Am I ever going to walk again? How am I going to stand up?’ I was alarmed about every strange mark on my body.
“Finally, I said, ‘Okay, Dorothy, you’ve got to control this cancer, the cancer is not going to control you.”
With time and healing, Dorothy became accustomed to her new normal as a melanoma survivor. She resumed working remotely. An occupational therapist taught her how to walk and safely perform daily tasks. She began walking on her toes, then gradually put pressure on her foot.
Educating People About the Dangers of Acral Melanoma
 While she was housebound, Dorothy considered writing a memoir about her experience. Then she decided to do something better: talk to people to educate them about acral melanoma and how to detect it. She was surprised at the lack of awareness about the disease.
While she was housebound, Dorothy considered writing a memoir about her experience. Then she decided to do something better: talk to people to educate them about acral melanoma and how to detect it. She was surprised at the lack of awareness about the disease.
“Every time I talked to someone about skin cancer on my foot, they’d look at me with their mouths open and say, ‘I’ve never heard such a thing,’” Dorothy explained.
Dorothy is also calling upon doctors to have representative photos in their offices. “Where are the pictures of cancer on black and brown skin in the doctor’s office? I’d like to see some pictures, so people can understand what it looks like.”
Dorothy held an awareness event at her church in June 2024. About 60 people attended, including dermatologists from the local hospital. Dorothy shared her story, the dermatologists performed free skin cancer screenings and held a skin cancer Q&A. Educational materials from The Skin Cancer Foundation were shared with participants.
“The response was overwhelming,” she said. “I’m here to educate. And I tell my story to anybody who wants to listen.”



Constant Vigilance
In the years since her surgery and recovery, Dorothy is diligent about getting checked.
“I’ve got everybody watching me,” she said. “I have scans every six months with my oncologist. I see the podiatrist every six to eight weeks, because he shaves off the scar tissue under my foot. My dentist looks in my mouth for anything unusual. My eye doctor looks in my eyes for melanoma.”
Dorothy performs monthly skin self-exams and checks her body for enlarged lymph nodes. She sees her dermatologist twice a year and sees her primary care physician regularly.
She works three days a week, and goes to the gym twice a week to keep the tissue in her foot alive. And Dorothy has made some style adjustments that involve protecting her skin from UV rays.
“I don’t wear nail polish or get pedicures anymore, because my oncologist explained symptoms that can show up under your nail bed,” she said. “I’m happy keeping my fingernails fresh, so I can recognize symptoms.”
Dorothy believes that people should take care of their bodies and be on the alert for anything suspicious: “If you see something new, changing or unusual on your body, on your hand on your feet; go to the doctor and ask ‘What’s this?’ If you can, get referred to a dermatologist.”
Join the #LoveYourSkin Campaign
To raise awareness about the dangers of skin cancer, we invite you to join our public awareness campaign — #LoveYourSkin — focused on skin cancer education, early detection and sun protection for skin of color.
It’s easy to get involved:
- Follow us on social media
- Share posts, facts and graphics to help spread the word (see below for some graphics to share)
- Use the hashtag #LoveYourSkinProtectYourSkin and tag us @SkinCancerOrg so we can amplify the message
- Hold an awareness event in your community. Dorothy distributed educational materials from The Skin Cancer Foundation. Contact us at [email protected] if you’d like to do the same!
Together, we can help one another, share the facts and the love. Because loving your skin means protecting your skin.
Download the Acral Melanoma Awareness Images