Basal Cell Carcinoma
Warning Signs & Pictures
What Does Basal Cell Carcinoma Look Like?
Understanding what basal cell carcinoma (BCC) looks like is important. With early detection and treatment, almost all basal cell skin cancers can be successfully removed without complications.
Look out for BCC warning signs, including new, changing or unusual skin growths, so you can spot skin cancers early, when they are easiest to treat and cure.
How to spot a BCC: five warning signs
Check for BCCs where your skin is most exposed to the sun, especially the face, ears, neck, scalp, chest, shoulders and back, but remember that they can occur anywhere on the body. Frequently, two or more of these warning signs and symptoms are apparent in a BCC tumor.
- An open sore that does not heal, and may bleed, ooze or crust. The sore might persist for weeks, or appear to heal and then come back.
- A reddish patch or irritated area, on the face, chest, shoulder, arm or leg that may crust, itch, hurt or cause no discomfort.
- A shiny bump or nodule that is pearly or clear, pink, red or white. The bump can also be pigmented (tan, black or brown), especially in people of color, and can be mistaken for a normal mole.
- A small pink growth with a slightly raised, rolled edge and a crusted indentation in the center that may develop tiny surface blood vessels over time.
- A scar-like area that is flat white, yellow or waxy in color. The skin appears shiny and taut, often with poorly defined borders. This warning sign may indicate an invasive BCC.
Basal cell carcinoma pictures. Please note: Since not all BCCs have the same appearance, these images serve as a general reference to what basal cell carcinoma looks like.
 An open sore that does not heal
An open sore that does not heal
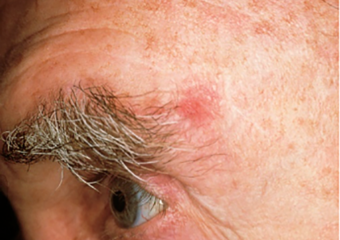 A reddish patch or irritated area
A reddish patch or irritated area
 A shiny bump or nodule
A shiny bump or nodule
 A scar-like area that is flat white, yellow or waxy in color
A scar-like area that is flat white, yellow or waxy in color
 A small pink growth with a slightly raised, rolled edge and a crusted indentation in the center
A small pink growth with a slightly raised, rolled edge and a crusted indentation in the center
 A basal cell carcinoma may be pigmented on skin of color. Photo: Andrew Alexis, MD, MPH
A basal cell carcinoma may be pigmented on skin of color. Photo: Andrew Alexis, MD, MPH
BCCs can be tricky
Keep in mind that BCCs can look different from the pictures and descriptions above. In some people, BCCs resemble noncancerous skin conditions such as psoriasis or eczema. In people with darker skin, about half of BCCs are pigmented (meaning brown in color).
When in doubt, check it out. Follow your instincts and visit your dermatologist if you see anything new, changing or unusual on your skin.
A basal cell carcinoma may be pigmented, like this one, on skin of color. Photo courtesy of Andrew Alexis, MD, MPH

What you can do
If you’ve already had a BCC, you are more likely to develop another, especially in the same sun-damaged area or nearby.
A BCC can recur even when it has been carefully removed the first time, because some cancer cells may remain undetectable after surgery and others can form roots that extend beyond what’s visible. BCCs on the nose, ears and lips are more likely to recur, usually within the first two years after surgery.
Here’s what you can do to detect a recurrence and prevent further skin damage that can lead to cancer:
- Be on the lookout: Pay particular attention to any previously treated site, note changes and consult with your dermatologist. If the BCC does return, your doctor may recommend a different type of treatment, such as Mohs surgery, a highly effective way to prevent and treat recurrences.
- Check yourself head to toe: Look for new or changing lesions that grow, bleed or do not heal. Learn how to check your skin.
- See your dermatologist annually for a professional skin exam. Self-exams do not take the place of a specialist who is skilled at identifying and treating abnormal skin growths.
- Follow up: If you’ve already had either BCC or squamous cell carcinoma (SCC), or a precancer like actinic keratosis, be sure to see your doctor at recommended intervals.
- Be sun-safe every day of the year: Avoid unprotected UV exposure, seek the shade, especially when the sun is strongest and use a broad-spectrum sunscreen, a wide-brimmed hat and UV-blocking sunglasses. Safeguarding yourself every day is the single most effective way to reduce your risk of developing skin cancer. Get more skin cancer prevention guidelines.
More BCC images
Reviewed by:
Julie K. Karen, MD
Ronald L. Moy, MD















