Mohs: The Gold Standard
By Arielle N.B. Kauvar, MD
Mohs surgery is on the rise, for good reasons: It has the lowest recurrence rates, highest cure rates and best cosmetic results of any skin cancer treatment. A physician member of The Skin Cancer Foundation explains why Mohs has it all.

Lifesaving new medications for people with advanced melanoma, called targeted therapies and immunotherapies, have grabbed the biggest skin cancer headlines in the past few years, and that’s good news. But for people with the more common nonmelanoma skin cancers, basal cell and squamous cell carcinoma (BCC and SCC), an older technique has also been drawing more attention and favor than ever. I recently led the task force to establish consensus guidelines on the treatment of BCC and SCC, which were published this year. They demonstrate that Mohs surgery is the treatment of choice for many BCCs and SCCS, and the single most precise and effective method for eliminating these cancers.1-3
Did you know your chance of developing a nonmelanoma skin cancer in your lifetime is about one in five? More than 5.3 million cases of BCC and SCC are diagnosed in the U.S. each year. Exposure to ultraviolet (UV) light, either from the sun or from indoor tanning, is the greatest risk factor for developing these skin cancers, so it’s not surprising that approximately 80 percent of these cancers occur on the head and neck, where exposure is greatest. Unfortunately, since these are the most conspicuous skin cancers, they are also the most cosmetically challenging, capable of becoming disfiguring and sometimes dangerous if not caught at an early stage.
That’s why I want you to know just what Mohs surgery is, how it works, and what it can do to leave you cancer-free while looking the best you can after surgery.
How Mohs surgery works
Sometimes known as Mohs micrographic surgery, the technique was invented in the 1930s by Dr. Frederic Mohs at the University of Wisconsin, but it didn’t develop into a mainstream treatment until practitioners such as NYU dermatologist Perry Robins, MD, refined the technique and spread the word about it in the 1970s and 1980s. The use of Mohs surgery has especially been growing in the past 15 years, above all for skin cancers in the head and neck region.2-5
The most obvious difference between Mohs surgery and routine excisional surgery is that Mohs is done in stages while you wait for lab results, which are obtained immediately on site, rather than the tissue sample being sent to a lab for results days later.
A surgeon specially trained in Mohs surgery, pathology and reconstructive surgery first may draw some marks around the lesion with ink to guide the treatment, then injects a local anesthesia. Using a scalpel, the doctor removes the thinnest possible layer of visible cancerous tissue. (Sometimes doctors gauge this by feel as well as by sight.) A nurse or assistant bandages your wound and shows you to a waiting area.
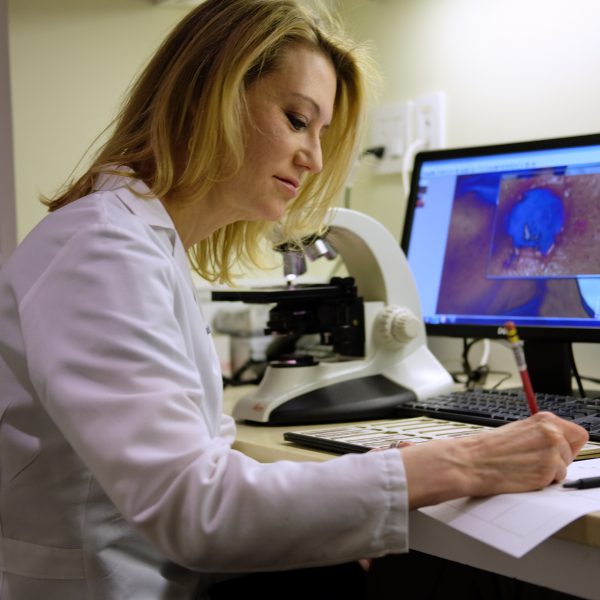
The surgeon then color-codes the tissue with ink to map exactly where it was removed from the body. Next, a technician processes the tumor in the on-site laboratory by freezing the tissue so that it can be readily cut into paper-thin sections (like a stack of dimes) and placed on slides. The tissue on the slides is then stained and the Mohs surgeon examines these slides under a microscope. If the doctor finds any remaining cancer cells, the areas are pinpointed on the map, and you’re called back into the operating room. The doctor numbs those areas again before precisely removing another layer of tissue from each of the locations where cancer cells remain.
Some Mohs surgery steps

Arielle Kauvar, MD, examines a cancerous area on the side of the patient’s nose.
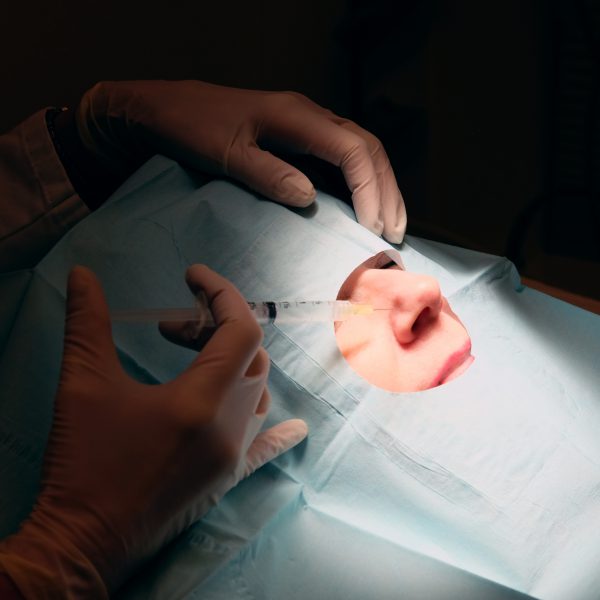
Before starting the surgery, Dr. Kauvar injects a local anesthetic.

Dr. Kauvar removes the first layer of cancerous tissue.

In the lab, the surgeon examines slides with sections of the removed tissue.
Next, she marks a map of where cancer cells remain before round two of surgery.

Bandaged, the patient waits for the lab results before another round of surgery. It takes time to get the all-clear, but it’s worth it!
The team repeats this whole process until the margins (edges) of the last excised tissue sample are clear and cancer-free. At that point, the doctor usually closes the wound with stitches. In some cases, a large wound on the face or around a joint may need reconstruction with a skin flap or a skin graft. Mohs surgeons are trained in these techniques, though in some cases, a plastic surgeon may do the reconstruction or closure. After that, the wound is bandaged, you’re given instructions on how to take care of the incision — and you’re done.
As you can imagine, all of this takes time. If you need several rounds, it may take several hours. But the time spent is worth it. The Mohs process examines 100 percent of the tissue margins under the microscope, whereas in standard surgical excision only 1 percent of the margins are examined microscopically. Mohs surgery also conserves the greatest amount of healthy tissue, giving you the smallest scar possible. The procedure is cost-effective because the cancer removal, microscopic evaluation and, in most cases, wound reconstruction are all done in one visit, and the cure rate is up to 99 percent.
Who should have Mohs?
Because of its high cure rate, Mohs surgery is now recommended as the treatment of choice for high-risk nonmelanoma skin cancers.1-3 Cancers on the nose, eyelids, lips, ears, hands, feet and genitals (some skin cancers are related to genetics or other causes rather than UV exposure) are all considered high-risk. Those on other areas of the face, scalp, neck and shins are considered intermediate risk.
Other skin cancers also best treated with Mohs surgery include:
- large cancers in normally low-risk areas.
- those with difficult-to-see borders.
- those with certain microscopic growth patterns.
- those that have recurred after initial treatment.
- those that could not be completely removed.
Mohs surgery is the front-line treatment for nonmelanoma skin cancers that grow in scar tissue or areas of prolonged inflammation, as well as skin that had previously been treated with radiation. Nonmelanoma skin cancers are also considered high-risk when they develop in patients whose immune systems are suppressed by medication (such as transplant recipients) or disease (such as leukemia), or in those with genetic syndromes that predispose them to skin cancers.
For small or superficial low-risk BCCs and SCCs on the abdomen, chest, back, arms and legs, standard treatments such as surgical excision, cryosurgery (freezing), curettage and electrodesiccation (scraping and burning), photodynamic therapy and topical medications may provide adequate therapy. (For more details on these procedures, see The Skin Cancer Foundation’s Treatment Glossary.)
Younger People Benefit, Too
The number of people who develop skin cancer has been increasing for decades, and, alarmingly, more women and men under age 40 are now being diagnosed with the disease. Particularly in women, indoor tanning has been linked by many experts to an increased incidence of skin cancers at younger ages.
In my practice, I treat at least one patient in his or her 30s each week with Mohs surgery and many in their 40s and 50s, which is vastly different than 20 years ago, when the majority of patients were older. Not many young people seriously worry about getting skin cancer. Many use tanning beds and skip sun protection, and if they discover an unusual growth on their skin, they often delay seeking treatment because they think it’s no big deal. But it can be. Basal cell carcinomas rarely metastasize, or spread through the body, but some have aggressive growth patterns and can cause significant damage by growing along nerves or blood vessels, or through muscle or bone. By allowing the cancer to grow, you risk requiring more extensive surgery in the future. Squamous cell carcinomas can be more dangerous, carrying an approximately 4 percent risk of metastasis and 2 percent risk of death6, and the risk increases when these cancers return after treatment.
That’s why it’s crucial for you to start as early as possible to protect yourself from the sun (see The Skin Cancer Foundation’s protection tips) and to start making a professional skin exam an annual habit. You should also check your own skin once a month head to toe, and get to a dermatologist immediately if you find any new or changing spot on your skin. It’s especially important to be aware that once you have had a skin cancer, you are at increased risk of one day developing new skin cancers elsewhere on the body.
It’s scary at any age to think about skin cancer surgery, especially when the cancer is on your nose, lips, ears or eyelids; it stirs up fears of scarring and disfigurement. Skin cancers in these critical locations have a high risk of recurring after treatment with standard techniques, and when they do recur they can require more extensive surgery because of undetected growth beneath the skin’s surface. Mohs surgery delivers the best cosmetic results, the lowest recurrence rate of any treatment method — and the highest chance of a complete cure. That’s good news at any age.
